
Pertinent medical history, surgical history (with year and surgeon if possible), family history, and social history is recorded. Subsequent visits for the same problem briefly summarize the HPI, including pertinent testing and results, referrals, treatments, outcomes and follow-ups.

It begins with the patient's age, sex, and reason for visit, and then the history and state of experienced symptoms are recorded.

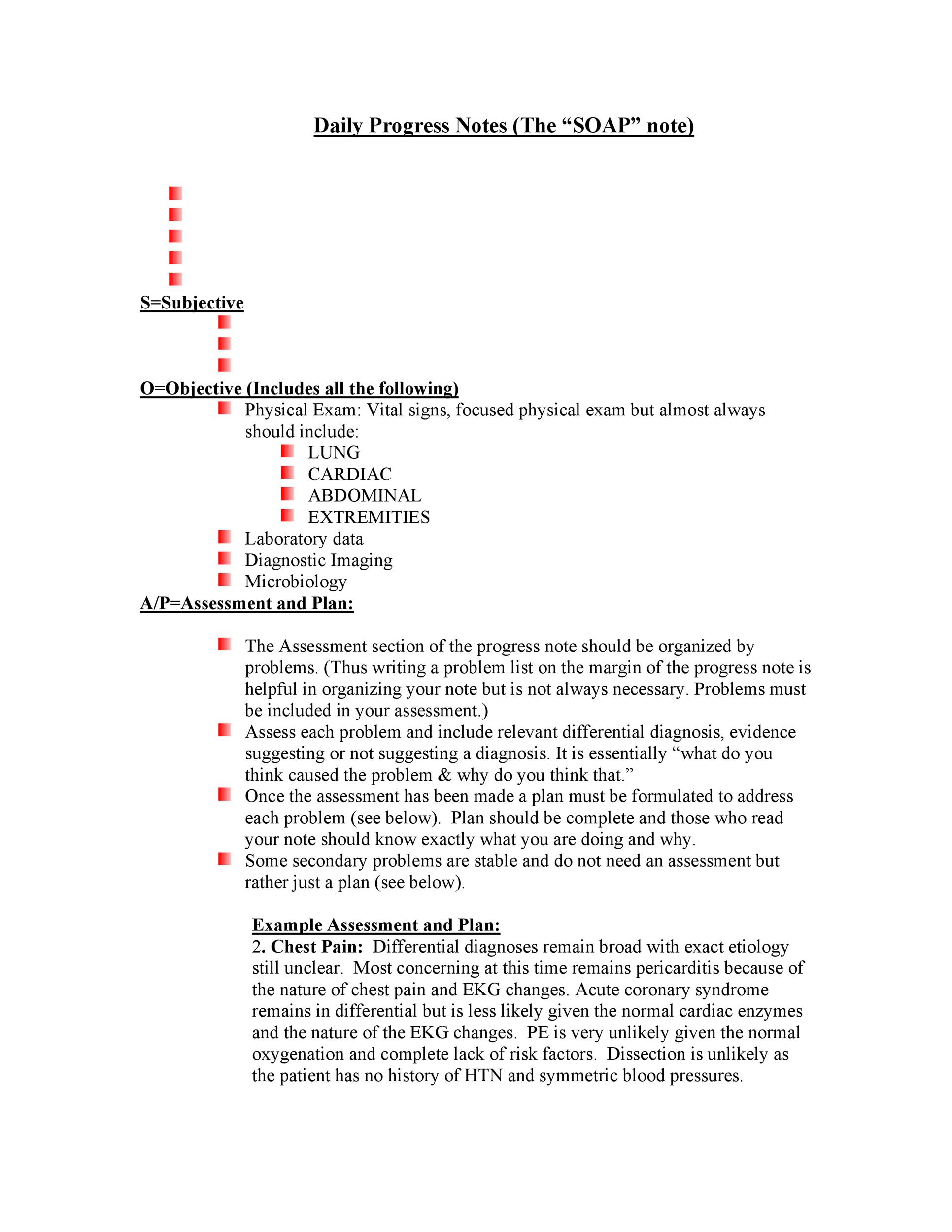
This describes the patient's current condition in narrative form, from the time of initial sign/symptom to the present. The physician will take a history of present illness, or HPI, of the CC. There can be multiple CC's, but identifying the most significant one is vital to make a proper diagnosis. The patient's chief complaint, or CC, is a very brief statement of the patient (quoted) as to the purpose of the office visit or hospitalization. Subjective component Chief Complaint (CC) The length and focus of each component of a SOAP note vary depending on the specialty for instance, a surgical SOAP note is likely to be much briefer than a medical SOAP note, and will focus on issues that relate to post-surgical status. The four components of a SOAP note are Subjective, Objective, Assessment, and Plan. Many healthcare providers, ranging from physicians to behavioral healthcare professionals to veterinarians, use the SOAP note format for their patient's initial visit and to monitor progress during follow-up care. Due to its clear objectives, the SOAP note provides physicians a way to standardize the organization of a patient's information to reduce confusion when patients are seen by various members of healthcare professionals. Prehospital care providers such as emergency medical technicians may use the same format to communicate patient information to emergency department clinicians. Generally, SOAP notes are used as a template to guide the information that physicians add to a patient's EMR. SOAP notes are commonly found in electronic medical records (EMR) and are used by providers of various backgrounds.

Today, it is widely adopted as a communication tool between inter-disciplinary healthcare providers as a way to document a patient's progress. It was initially developed for physicians to allow them to approach complex patients with multiple problems in a highly organized way.
The SOAP note originated from the problem-oriented medical record (POMR), developed nearly 50 years ago by Lawrence Weed, MD. Additionally, it serves as a general cognitive framework for physicians to follow as they assess their patients. Documenting patient encounters in the medical record is an integral part of practice workflow starting with appointment scheduling, patient check-in and exam, documentation of notes, check-out, rescheduling, and medical billing. The SOAP note (an acronym for subjective, objective, assessment, and plan) is a method of documentation employed by healthcare providers to write out notes in a patient's chart, along with other common formats, such as the admission note.


 0 kommentar(er)
0 kommentar(er)
